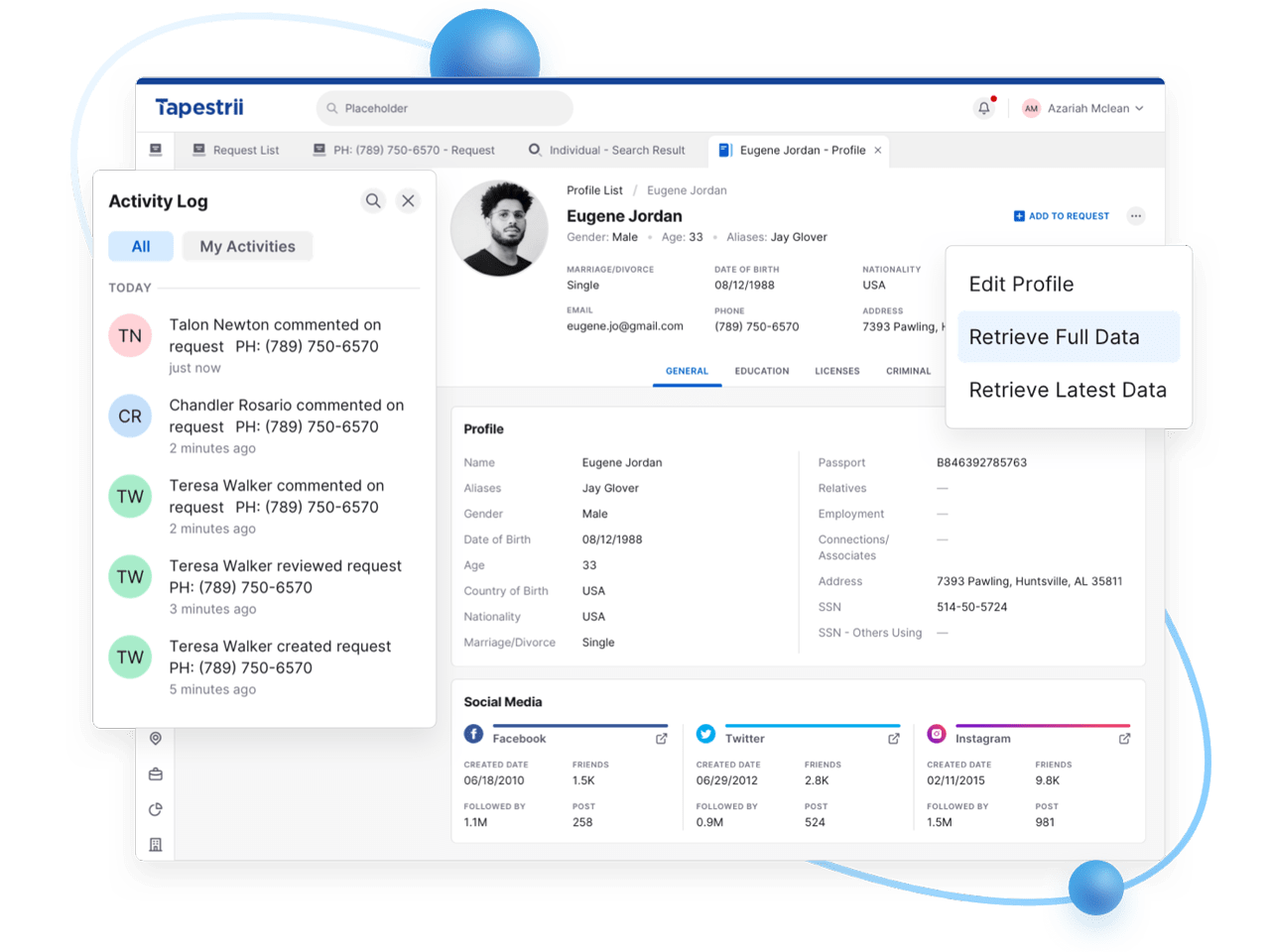
The client provides technology solutions for the Healthcare industry in processing patient enrollment, benefit plan administration, and claims processing for third-party administrators and account care organizations throughout hospital systems nationwide.
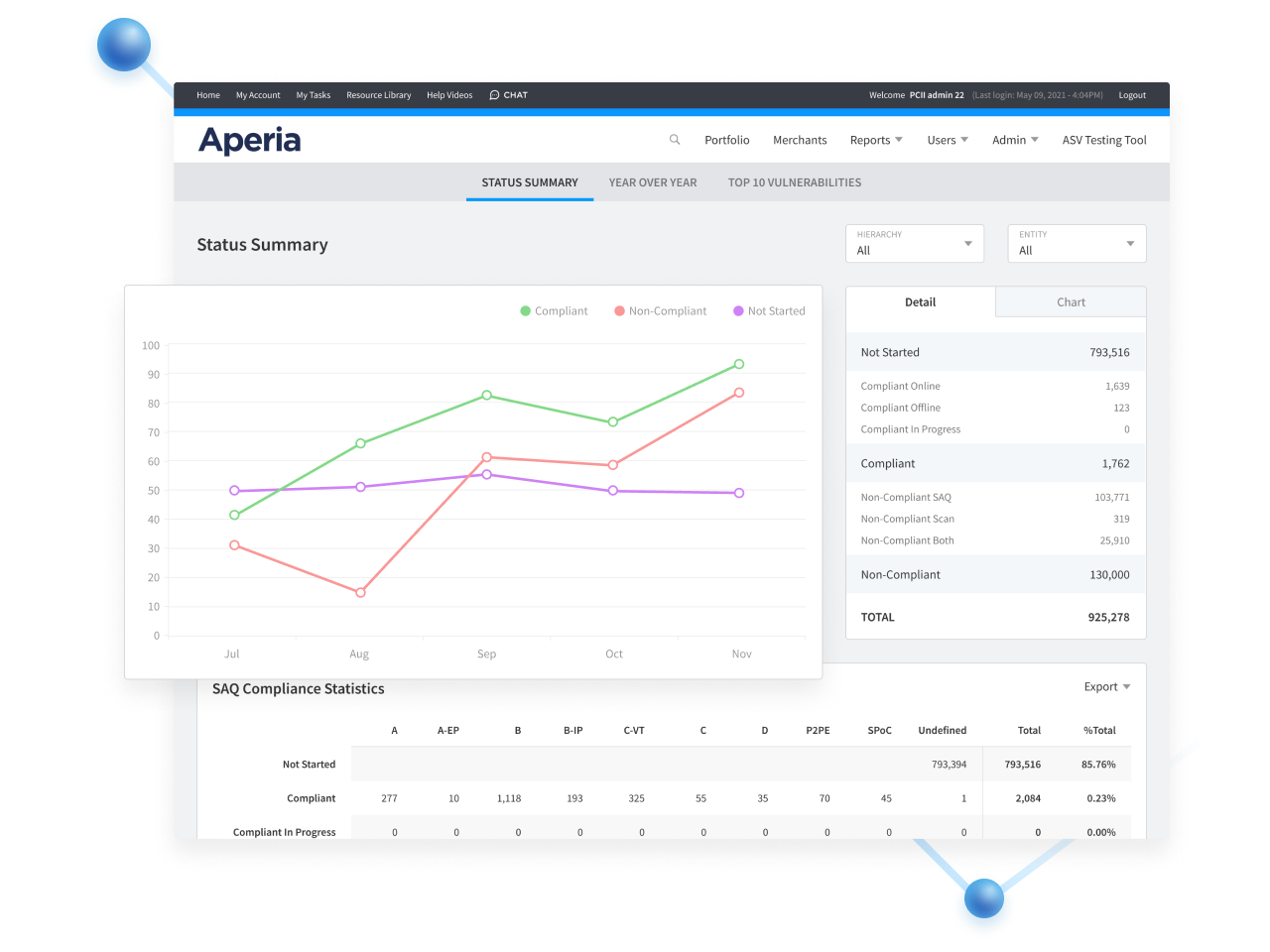
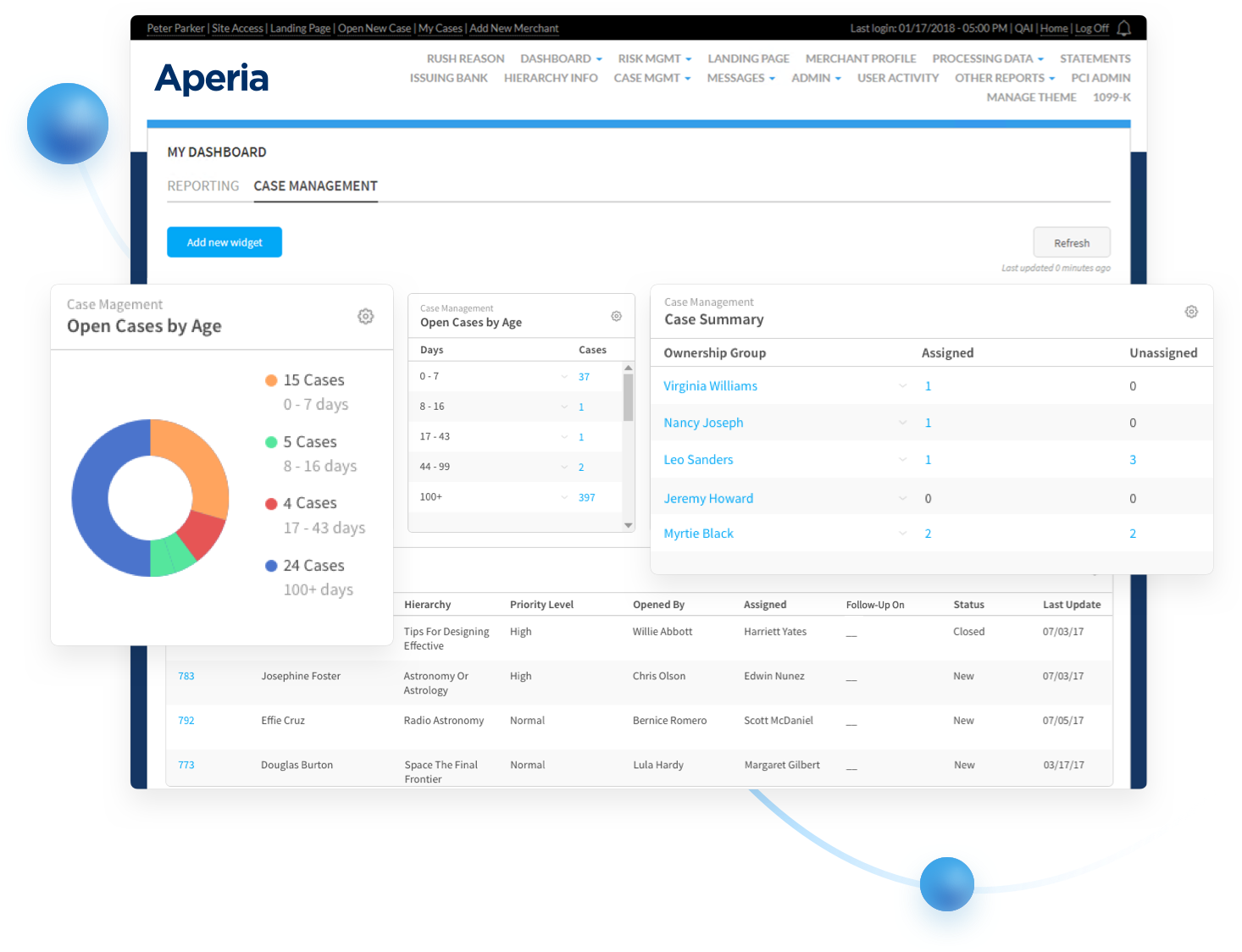
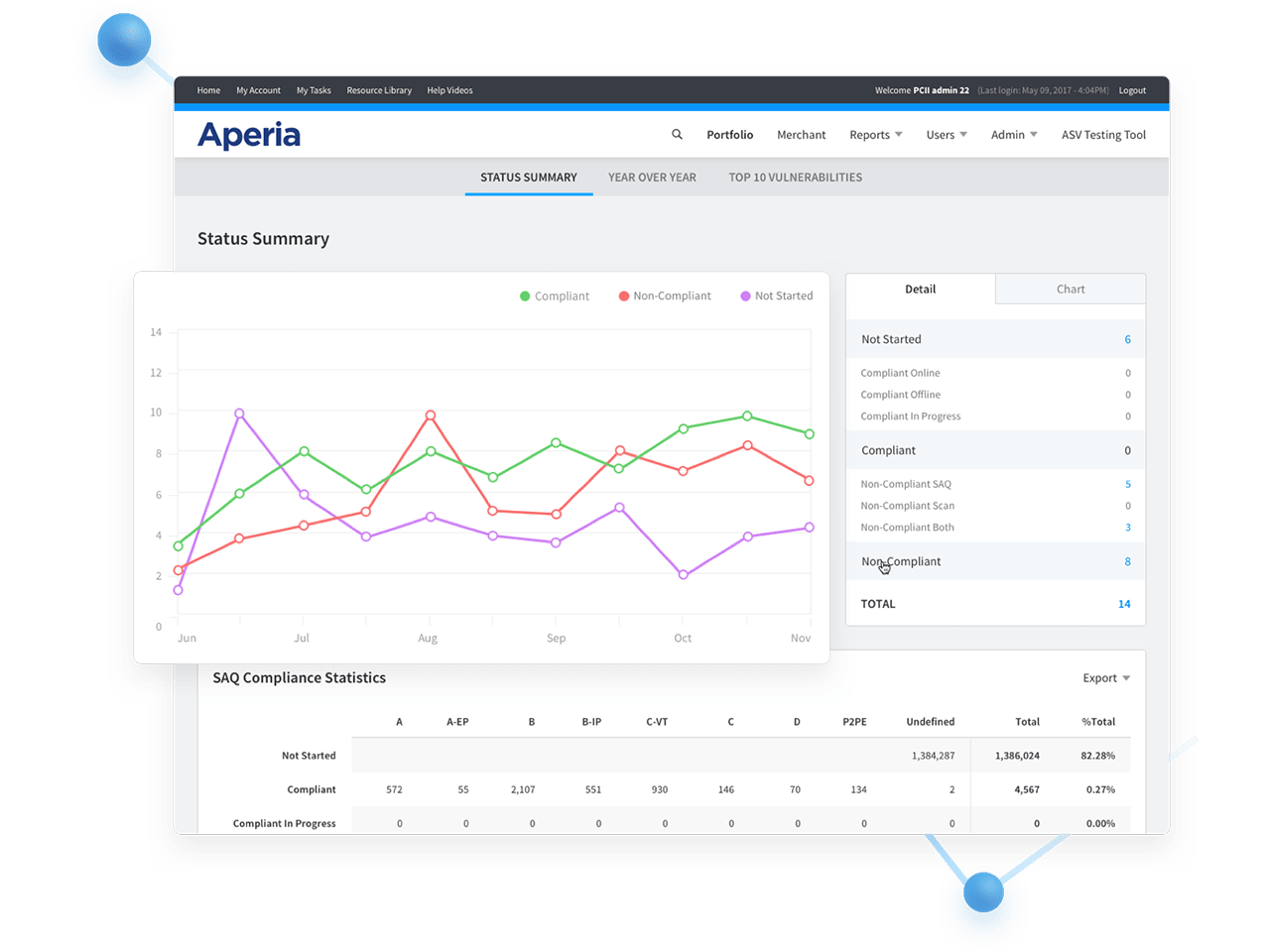
Aperia developed a solution that dynamically ingests and monitors inbound files, generates processing statistics, normalizes data through a rules-based validation engine, and ensures complete and accurate output. Claims processing time dropped from 120 minutes to 8 minutes. We scoped, designed, and delivered the solution in four weeks and at half the cost of other bids.